How to examine patients and report findings in patients with suspected muscle diseases:
- Abnormal movements
- Fasciculation → peripheral nerve injury
- Tremor
- Resting → Parkinsonism (with bradykinesia and rigidity)
- Intention → cerebellar issue → look for additional signs of cerebellar problems (e.g., ataxia)
- Myoclonus (involuntary purposeless jerks of limbs) → toxic metabolic issues (e.g., hypoxia, uremia, serotonin syndrome, opioid intoxication) or upper motor neuron lesion
- Muscle tone
- Flaccid → lower motor neuron lesion or hyperacute CNS lesion (brain, spinal cord)
- Normal → myopathy
- Increased → dystonia
- Spastic → lower motor neuron lesion
- Rigid
- Parkinsonism
- Neuroleptic malignant syndrome
- Impaired relaxation = myotonia
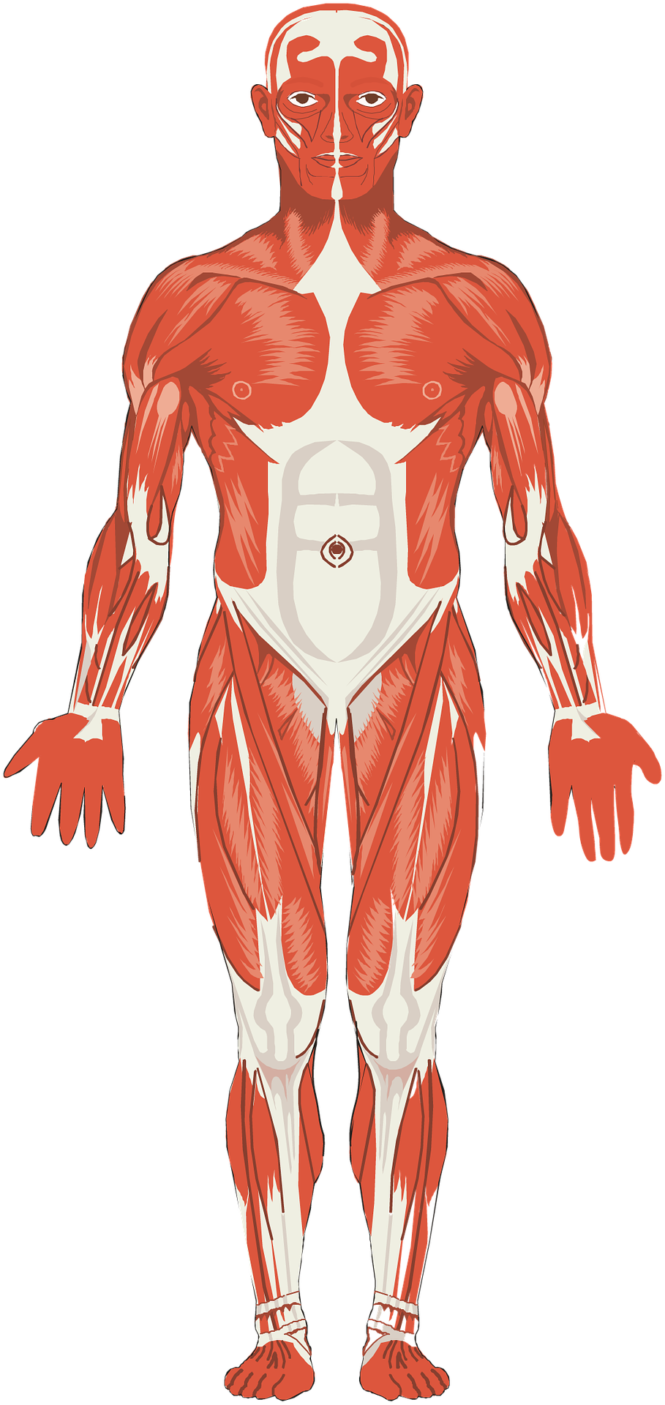
- Muscle Bulk
- Decreased (atrophy) → lots of things can cause this
- Deconditioning
- Cachexia
- Motor neuron disease
- Muscular dystrophy
- Normal → neuromuscular junction diseases or early inflammatory myopathies
- Hypertrophic (bulky and strong) → physical conditioning, anabolic steroid use
- Pseudohypertrophic (bulky and weak) → muscular dystrophies
- Decreased (atrophy) → lots of things can cause this
- Muscle tenderness
- Rhabdomyolysis
- Also, sometimes seen in myopathies
- Power, strength
- Diminished → myopathy, especially when proximal
- Fatigability → hallmark of myasthenia gravis
- Increased → physical conditioning, anabolic steroid use
- Muscle stretch reflexes (deep “tendon” reflexes)
- Diminished or absent → Lower motor neuron disease, late stages of myopathies
- Delayed upstroke → Hypothyroid myopathy
- Normal → Early stages of most myopathies
- Hyperreflexia
- Thyrotoxic myopathy
- Serotonin syndrome
- Upper motor neuron disease (remember: hyper goes with upper, while diminished or absent goes with lower)
- Gait
- Waddling (myopathic) gait → pelvis tilts downward on the side of the limb that is in the air (secondary to weakness in hip abductor muscles) resulting in side-to-side tilting of pelvis (waddling) with each step.
Watch this excellent one and half minute YouTube video which demonstrates and explains the myopathic gait:
Reference
- Neurology: A Clinician’s Approach (2010)

Leave a Reply