Category: Neurology
-
Raven Neurology Review: For the Medical Student Clerkship (2018)
Raven Neurology Review: For the Medical Student Clerkship (2018) is an excellent clinical neurology book that is geared toward intermediate-level medical students, particularly those who are taking a neurology clerkship or studying for the shelf examination. Presentations are mostly case-based. For example, the book (page 135) provides a case of a young female with obesity…
-
Fenichel’s Clinical Pediatric Neurology (2019)
Fenichel’s Clinical Pediatric Neurology (2019) is principally for pediatricians and neurologists, but there are very good reasons why generalists should have a good look at this book as well: it’s well organized in its clinical approach and will help you learn how to solve clinical problems in other fields too. Take, for example, hexosaminidase A…
-
Neurology: A Clinician’s Approach (2016)
The idea behind Neurology: A Clinician’s Approach (2016) … is to group diseases in the way in which they appear clinically…. I recommend it to more advanced rotating third and fourth year medical students, particularly those with a serious interest in internal medicine, neurology or neurosurgery.
-
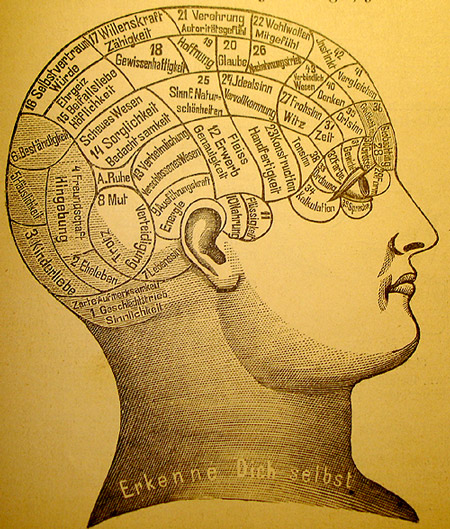
Why Consciousness is Not a Hard Problem
The “Hard Problem” Consciousness seems like a very difficult and vexing problem to many. The problem, variously phrased, can be stated this way: in a universe that is so obviously full of things that are objectively observable, how is it possible for there to be a purely subjective, first person experience that only I can…
-
Ataxia: The Physical Examination
Ataxia is an extremely important clinical sign that has a broad and important differential diagnosis. Causes of ataxia include posterior circulation strokes and various toxic and metabolic insults to the cerebellum (and sometimes to the spinocerebellar tracts). Ataxia can be a very subtle physical finding, especially when you don’t know what to look for or…
-
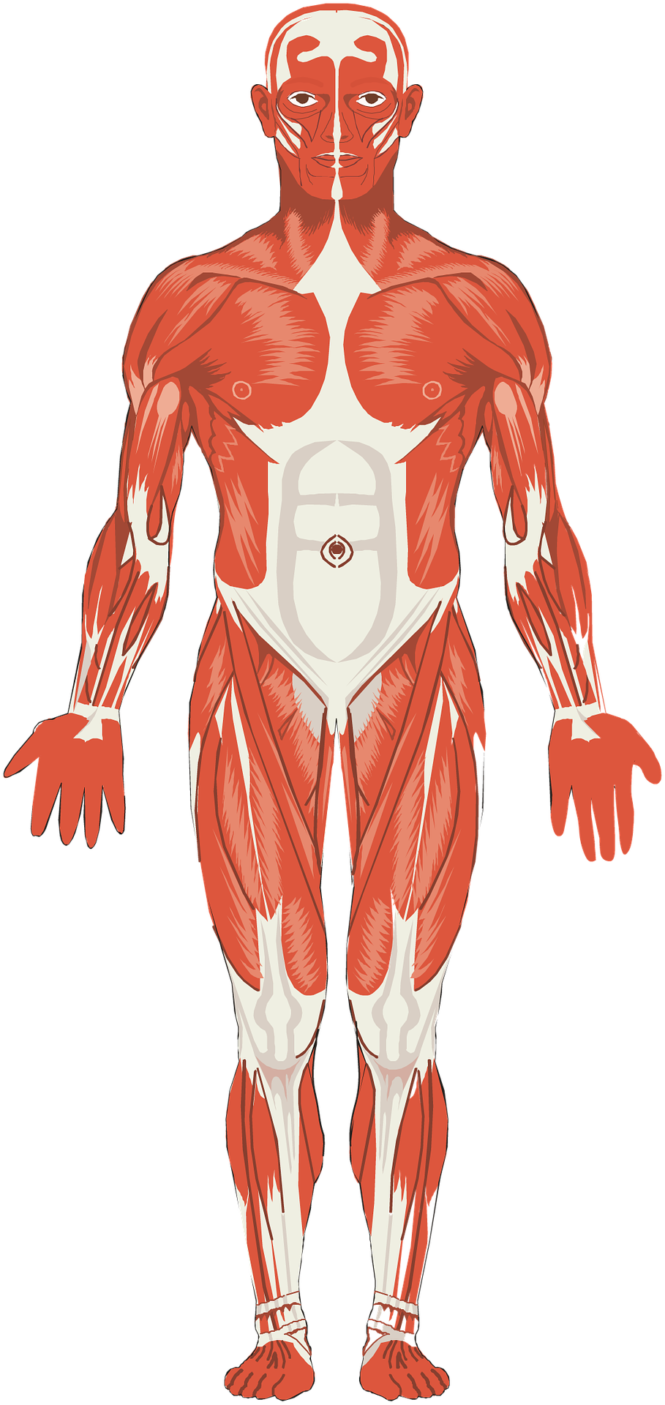
Physical Examination of Muscles in Systemic Disease
How to examine patients and report findings in patients with suspected muscle diseases: Abnormal movements Fasciculation → peripheral nerve injury Tremor Resting → Parkinsonism (with bradykinesia and rigidity) Intention → cerebellar issue → look for additional signs of cerebellar problems (e.g., ataxia) Myoclonus (involuntary purposeless jerks of limbs) → toxic metabolic issues (e.g., hypoxia, uremia,…
-
Central vs. Peripheral Vertigo Simplified
The first and most important step in evaluating a patient with vertigo is to attempt to distinguish vertigo of central origin from vertigo of peripheral origin because the management of central vertigo (brain imaging, hospital admission) is very different from the management of peripheral vertigo (symptomatic treatment, outpatient referral). Differences Between Central and Peripheral Vertigo Peripheral Vertigo…